By Fox Chase Cancer Center, New research suggests that men with prostate cancer who choose radiation therapy should seek treatment centers that will offer high-dose radiation. A new study from Fox Chase Cancer Center finds that higher doses of 74 to 82 Gray (Gy) greatly reduce the risk that the cancer will spread later--even 8-10 years after treatment.
"There is a comprehensive body of evidence demonstrating that prostate cancer treated with higher doses of radiation is less likely to grow back in the prostate or cause a rising PSA, and now, we know it is also less likely to spread later to other parts of the body," explained Peter Morgan, M.D., a resident in the Radiation Oncology Department at Fox Chase Cancer Center.
Generally, treatment centers that offer 3D conformal radiation therapy or a newer system of radiation delivery called IMRT (intensity modulated radiation therapy) treat men with the higher levels of radiation shown in this study to prevent the cancer's spread.
Morgan said that no published data from prospective randomized trials have shown a significant reduction in distant metastasis with higher radiation dose, likely because patients have not been followed for long enough to see the reduced of late-wave of metastasis. The current study shows that the risk of cancer spreading 8-10 years after treatment is lower when doses >74 Gray of radiation are given.
When asked how more radiation to the prostate protects the rest of the body from the cancer, Dr. Morgan replied, "That's what is so important about this work. We believe that the late wave of distant metastasis is due to the persistence of cancer in the prostate itself, which subsequently seeds tumor cells to other parts of the body. Because higher dose radiation more effectively kills cancer in the prostate, the source for future metastases is eliminated."
From 1989 to 1999, 667 men with intermediate- to high-risk prostate cancer were treated consecutively with 3D conformal radiation therapy. The outcomes of men who received less than 74 Gy, 74-75.9 Gy and greater than 76 Gy were compared. These groups had a median follow-up of 84, 84 and 65 months, respectively. The 10-year rate of the cancer spreading outside of the prostate (distant metastasis) was 16 percent for radiation doses less than 74 Gy, 7 percent for 74-75.9 Gy, and 3 percent for greater than 76 Gy.
Morgan said, "At our institution the policy for several years has been to treat prostate cancer to a dose of 76 to 80 Gy using IMRT. This study confirms that we are doing the right thing."
- The results of the study were presented today at the 48th Annual Meeting of the American Society for Therapeutic Radiology and Oncology in Philadelphia.
Saturday, December 02, 2006
Tea Soothes Skin Damage Linked to Cancer Treatment
Tea extracts can help reduce skin damage caused by cancer radiation therapy, according to a study by American and German researchers.
They examined the effects of green tea and black tea extracts and found that they reduced the duration of radiation-induced skin damage by five to 10 days. The tea extracts work at the cellular level to inhibit inflammatory pathways and reduce inflammation, said the team from the University of California, Los Angeles, and the University of Freiburg.
As well as testing the extracts on patients, the researchers studied the effects of green and black tea extracts on human and mouse white blood cells in laboratory cell cultures.
They found that the extracts reduced the release of pro-inflammatory cytokines, such as IL-1beta, IL-6, IL-8, TNF-alpha and PGE2, in human white blood cells. Green tea extract appeared to have higher anti-inflammatory properties than black tea extract.
Both green and black tea extracts inhibited one major inflammatory pathway in mouse white blood cells.
The researchers said that the high amount of polyphenols in tea is likely responsible for its anti-inflammatory activity, but added that other pathways are likely involved in its clinical effectiveness.
The study is published in the journal BMC Medicine.
They examined the effects of green tea and black tea extracts and found that they reduced the duration of radiation-induced skin damage by five to 10 days. The tea extracts work at the cellular level to inhibit inflammatory pathways and reduce inflammation, said the team from the University of California, Los Angeles, and the University of Freiburg.
As well as testing the extracts on patients, the researchers studied the effects of green and black tea extracts on human and mouse white blood cells in laboratory cell cultures.
They found that the extracts reduced the release of pro-inflammatory cytokines, such as IL-1beta, IL-6, IL-8, TNF-alpha and PGE2, in human white blood cells. Green tea extract appeared to have higher anti-inflammatory properties than black tea extract.
Both green and black tea extracts inhibited one major inflammatory pathway in mouse white blood cells.
The researchers said that the high amount of polyphenols in tea is likely responsible for its anti-inflammatory activity, but added that other pathways are likely involved in its clinical effectiveness.
The study is published in the journal BMC Medicine.
Thursday, November 16, 2006
Sunday, October 29, 2006
Palliation
Life is an ongoing challenge. To deal with terminal patients on a continuous basis requires strength. Fungated post penectomy inguinal mass, a post operated carcinoma prostate-bleeding for more than 12 hours, a Carcinoma lung with metastasis to almost the complete spine, a unknown primary with carcinomatous meningitis and multiple metastasis, etc etc.
Few get palliated and few don't. It is our duty to do the best to them.
The penectomy patient has improved after palliative radiation.
The prostate patient's relatives were not ready to spend. Inspite of me offering radiation at free of cost to them, they were not ready to get the required blood to support him. His hemoglobin was less than 4 gm%.
The patient got discharged without any treatment and I felt a tinge of regret. The inevitable must have happened.
There was another patient referred from my alma mater 'Tata Memorial Hospital', Carcinoma lung with brain metastases. The patient was in good shape. The sons decided to only offer Steroid medication as supportive care to their dad, fearing that radiation is painful. Both sons were well educated but decided to go against a treatment which would have improved thier dad's life as well as given him a better quality of life.
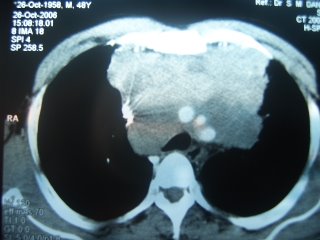
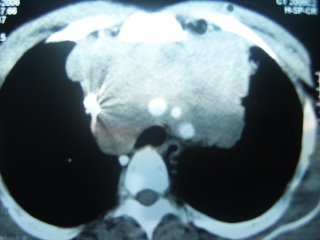
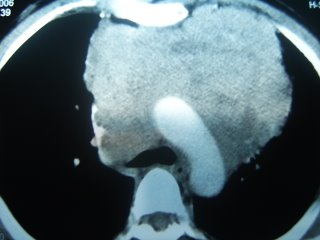
At present there is another patient of carcinoma lung admitted, who has multiple vertebral metastasis. His pain due to metastasis has reduced but he still continues to be breathless. He has bilateral lung infiltrates. Everyday is a challenge to treat him.
Few get palliated and few don't. It is our duty to do the best to them.
The penectomy patient has improved after palliative radiation.
The prostate patient's relatives were not ready to spend. Inspite of me offering radiation at free of cost to them, they were not ready to get the required blood to support him. His hemoglobin was less than 4 gm%.
The patient got discharged without any treatment and I felt a tinge of regret. The inevitable must have happened.
There was another patient referred from my alma mater 'Tata Memorial Hospital', Carcinoma lung with brain metastases. The patient was in good shape. The sons decided to only offer Steroid medication as supportive care to their dad, fearing that radiation is painful. Both sons were well educated but decided to go against a treatment which would have improved thier dad's life as well as given him a better quality of life.
At present there is another patient of carcinoma lung admitted, who has multiple vertebral metastasis. His pain due to metastasis has reduced but he still continues to be breathless. He has bilateral lung infiltrates. Everyday is a challenge to treat him.
Friday, October 06, 2006
Peripheral Radiotherapy Center
I have moved from Tata Memorial Hospital to a peripheral Cancer center. It is entirely different experience to discuss issues with patient and counsel them as an independent doctor. I am learning each day.
I have a tough 60 year old gentleman suffering from multiple myeloma. He has visited a tertiary care center at Bangalore and is not happy with the whole experience. He is not interested in any kind of treatment and is preently in a denial mode.
I have at present just promised to relieve his pain. I hope he improves with pain relief and get backs for further treatment.
I have a tough 60 year old gentleman suffering from multiple myeloma. He has visited a tertiary care center at Bangalore and is not happy with the whole experience. He is not interested in any kind of treatment and is preently in a denial mode.
I have at present just promised to relieve his pain. I hope he improves with pain relief and get backs for further treatment.
Wednesday, August 02, 2006
Wednesday, May 24, 2006
Wednesday, April 05, 2006
Breast Cancer Quality of Life(QOL)
Weight training improves quality of life (QOL) in breast cancer survivors, according to the results of a randomized trial reported in the March 27 Early View issue of Cancer.
"Aerobic exercise training has been shown to have beneficial effects on QOL in breast cancer survivors," write Tetsuya Ohira, MD, from the University of Minnesota in Minneapolis, and colleagues from the Weight Training for Breast Cancer Survivors (WTBS) Study. "However, the effects of weight training on psychological benefits are unknown.... There is the potential that for breast cancer survivors, weight training might increase a sense of control over their lives during the 'watchful waiting' time frame between the end of active treatment and the 5-year mark post-diagnosis (e.g., psychological empowerment via physical strength increases)."
Aerobic exercise has been demonstrated to improve a variety of outcomes among women who survive breast cancer, from fatigue to depression and QOL. An analysis of the Nurses' Health Study by Holmes and colleagues, which was published in the May 25, 2005, issue of JAMA, examined the risk for mortality associated with various levels of physical activity among breast cancer survivors. The authors found that walking 3 to 5 hours per week at an average pace could significantly reduce the risk for all-cause mortality compared with walking less than 3 hours per week. There was little additional survival benefit for more intense exercise regimens.
"Aerobic exercise training has been shown to have beneficial effects on QOL in breast cancer survivors," write Tetsuya Ohira, MD, from the University of Minnesota in Minneapolis, and colleagues from the Weight Training for Breast Cancer Survivors (WTBS) Study. "However, the effects of weight training on psychological benefits are unknown.... There is the potential that for breast cancer survivors, weight training might increase a sense of control over their lives during the 'watchful waiting' time frame between the end of active treatment and the 5-year mark post-diagnosis (e.g., psychological empowerment via physical strength increases)."
Aerobic exercise has been demonstrated to improve a variety of outcomes among women who survive breast cancer, from fatigue to depression and QOL. An analysis of the Nurses' Health Study by Holmes and colleagues, which was published in the May 25, 2005, issue of JAMA, examined the risk for mortality associated with various levels of physical activity among breast cancer survivors. The authors found that walking 3 to 5 hours per week at an average pace could significantly reduce the risk for all-cause mortality compared with walking less than 3 hours per week. There was little additional survival benefit for more intense exercise regimens.
Friday, March 31, 2006
Oral side effects of Radiotherapy
Taken from Lancet Oncology
Because of typical tissue reactions to ionising radiation, radiotherapy in the head and neck region usually results in complex oral complications aff ecting the salivary glands, oral mucosa, bone, masticatory musculature, and dentition. When the oral cavity and salivary glands are exposed to high doses of radiation, clinical consequences including hyposalivation, mucositis, taste loss, trismus, and osteoradionecrosis should be regarded as the most common side-eff ects. Mucositis and taste loss are reversible consequences, usually subsiding early post-irradiation,
whereas hyposalivation is commonly irreversible. Additionally, the risk of rampant tooth decay with its sudden onset and osteonecrosis is a lifelong threat. Thus, early, active participation of the dental profession in the development of preventive and therapeutic strategies, and in the education and rehabilitation of patients is paramount in consideration of quality-of-life issues during and after radiotherapy.
Because of typical tissue reactions to ionising radiation, radiotherapy in the head and neck region usually results in complex oral complications aff ecting the salivary glands, oral mucosa, bone, masticatory musculature, and dentition. When the oral cavity and salivary glands are exposed to high doses of radiation, clinical consequences including hyposalivation, mucositis, taste loss, trismus, and osteoradionecrosis should be regarded as the most common side-eff ects. Mucositis and taste loss are reversible consequences, usually subsiding early post-irradiation,
whereas hyposalivation is commonly irreversible. Additionally, the risk of rampant tooth decay with its sudden onset and osteonecrosis is a lifelong threat. Thus, early, active participation of the dental profession in the development of preventive and therapeutic strategies, and in the education and rehabilitation of patients is paramount in consideration of quality-of-life issues during and after radiotherapy.
Wednesday, March 15, 2006
RADIOTHERAPY IN BREAST CANCER
In Breast Conserving Surgery patients;
After breast-conserving surgery (BCS), a particularly common site of local recurrence is the conserved breast itself (or the axilla, if this has not been treated effectively). The risk of recurrence in a conserved breast can be substantial even in node-negative disease that has
been confirmed by axillary clearance, and it can be greatly reduced by radiotherapy. Hence, the recent National Institutes of Health (NIH) consensus conference on early breast cancer recommended that after BCS there should be radiotherapy to the conserved breast.
Post-mastectomy radiotherapy:
Even after mastectomy, an appreciable risk of local recurrence (eg, in the chest wall or lymph nodes) can remain unless some reliable method of investigation, such as axillary clearance, has found no evidence of nodal involvement. If axillary investigation reveals nodal involvement (or if the axilla has not been adequately investigated), post-mastectomy radiotherapy can produce
a substantial absolute reduction in this risk of local recurrence, and previous trials and meta-analyses have shown that although it has little effect on breast cancer mortality during the first few years, it can produce a moderate, but definite, reduction in longer-term breast
cancer mortality. Hence, the NIH consensus conference recommended radiotherapy after mastectomy for women at high risk of locoregional recurrence (eg, those with four or more involved lymph nodes).
Any doubts or queries, you can mail or leave your question here.
After breast-conserving surgery (BCS), a particularly common site of local recurrence is the conserved breast itself (or the axilla, if this has not been treated effectively). The risk of recurrence in a conserved breast can be substantial even in node-negative disease that has
been confirmed by axillary clearance, and it can be greatly reduced by radiotherapy. Hence, the recent National Institutes of Health (NIH) consensus conference on early breast cancer recommended that after BCS there should be radiotherapy to the conserved breast.
Post-mastectomy radiotherapy:
Even after mastectomy, an appreciable risk of local recurrence (eg, in the chest wall or lymph nodes) can remain unless some reliable method of investigation, such as axillary clearance, has found no evidence of nodal involvement. If axillary investigation reveals nodal involvement (or if the axilla has not been adequately investigated), post-mastectomy radiotherapy can produce
a substantial absolute reduction in this risk of local recurrence, and previous trials and meta-analyses have shown that although it has little effect on breast cancer mortality during the first few years, it can produce a moderate, but definite, reduction in longer-term breast
cancer mortality. Hence, the NIH consensus conference recommended radiotherapy after mastectomy for women at high risk of locoregional recurrence (eg, those with four or more involved lymph nodes).
Any doubts or queries, you can mail or leave your question here.
Thursday, March 09, 2006
Effective Palliation and Medical Records
The tongue cancer patient from Indore did visit me today. She was operated in May and took radiation after surgery. They had brought lot of medical documents but only few had relevant information.
I could not make out from the records what was her pre therapy staging, what kind of operation was done etc. From the histopathology I learnt that the cancer was of squamous cell type infiltrating one-third of tongue. The radiotherapy paper let me know that she has received 6000cGy. Apart from this there was no greater detail.
I could not decipher why a neck dissection was not done and why even though the patient was on regular follow up the neck node was allowed to grow to a size of cricket ball. The surgeon at Indore , supposed to be very reputed and above 60 years, adviced endoscopy for her complaint of inability to swallow. His attention on side effects of radiotherapy prevented him from addressing the neck nodes. Ofcourse I counselled the patients that the treatment at Indore was appropriate and the situation is bad becuse biologically the tumor is bad.
The patient had come with great hopes of getting treated at Mumbai but as she is having advanced malignancy,because of a large matted neck node engulfing the carotid , I adviced them palliative care at Indore itself. It is much better to be at home and take treatment than to struggle in an alien city. I tried to guide them to the best. Hope they heed my advice and take supportive care at Indore or at the maximum palliative cisplatin based chemotherapy.
I could not make out from the records what was her pre therapy staging, what kind of operation was done etc. From the histopathology I learnt that the cancer was of squamous cell type infiltrating one-third of tongue. The radiotherapy paper let me know that she has received 6000cGy. Apart from this there was no greater detail.
I could not decipher why a neck dissection was not done and why even though the patient was on regular follow up the neck node was allowed to grow to a size of cricket ball. The surgeon at Indore , supposed to be very reputed and above 60 years, adviced endoscopy for her complaint of inability to swallow. His attention on side effects of radiotherapy prevented him from addressing the neck nodes. Ofcourse I counselled the patients that the treatment at Indore was appropriate and the situation is bad becuse biologically the tumor is bad.
The patient had come with great hopes of getting treated at Mumbai but as she is having advanced malignancy,because of a large matted neck node engulfing the carotid , I adviced them palliative care at Indore itself. It is much better to be at home and take treatment than to struggle in an alien city. I tried to guide them to the best. Hope they heed my advice and take supportive care at Indore or at the maximum palliative cisplatin based chemotherapy.
Wednesday, March 08, 2006
Tongue cancer
Today morning I got a phone call from a patient at Nashik. The patient is a female less than 40 years of age who has been treated for tongue cancer at Indore. She was operated at Indore and also took post operative Radiotherapy at Indore itself. At present her complaints are that she is not able to take even liquids properly. She has been investigated at Nashik and the doctor over there opined that it is a recurrence which is not salvageable. She has been offered palliative chemotherapy. They also have been given an impression that if chemotherapy would have been given after surgery then she had a better chance of disease control.
The lady is coming tomorrow for consultation to Mumbai. i will get a better summary of the case tomorrow.
The problems she is facing can be due to Radiotherapy or because of tumor recurrence. If it is a tumor recurrence it is bad for her.
i wanted to tell them that it is going to be a futile attempt coming to Mumabi as Indore also has excellent doctors. Also the second opinion in this treated case probably is not going to change much for her. But who am I to deny hope. They will feel better after they have consulted a premier hospital at Mumbai.
Let hope prevail.
The lady is coming tomorrow for consultation to Mumbai. i will get a better summary of the case tomorrow.
The problems she is facing can be due to Radiotherapy or because of tumor recurrence. If it is a tumor recurrence it is bad for her.
i wanted to tell them that it is going to be a futile attempt coming to Mumabi as Indore also has excellent doctors. Also the second opinion in this treated case probably is not going to change much for her. But who am I to deny hope. They will feel better after they have consulted a premier hospital at Mumbai.
Let hope prevail.
Wednesday, March 01, 2006
Subscribe to:
Comments (Atom)